Chronic Pain, Depression & Covid 19
The relation between chronic pain with anxiety and/or depression
Many studies proved that there is a strong association between chronic pain and depression. Depression can cause different types of pain called somatization and on the opposite hand chronic pain can cause anxiety and depression. In several studies, this association has been found in greater than 50% of cases. Many patients with chronic pain have noticed this association and that they frequently complain of increased feelings of pain once they are depressed for other family reasons or personal reasons.
How is the psychological status of patients with chronic pain in Covid time?
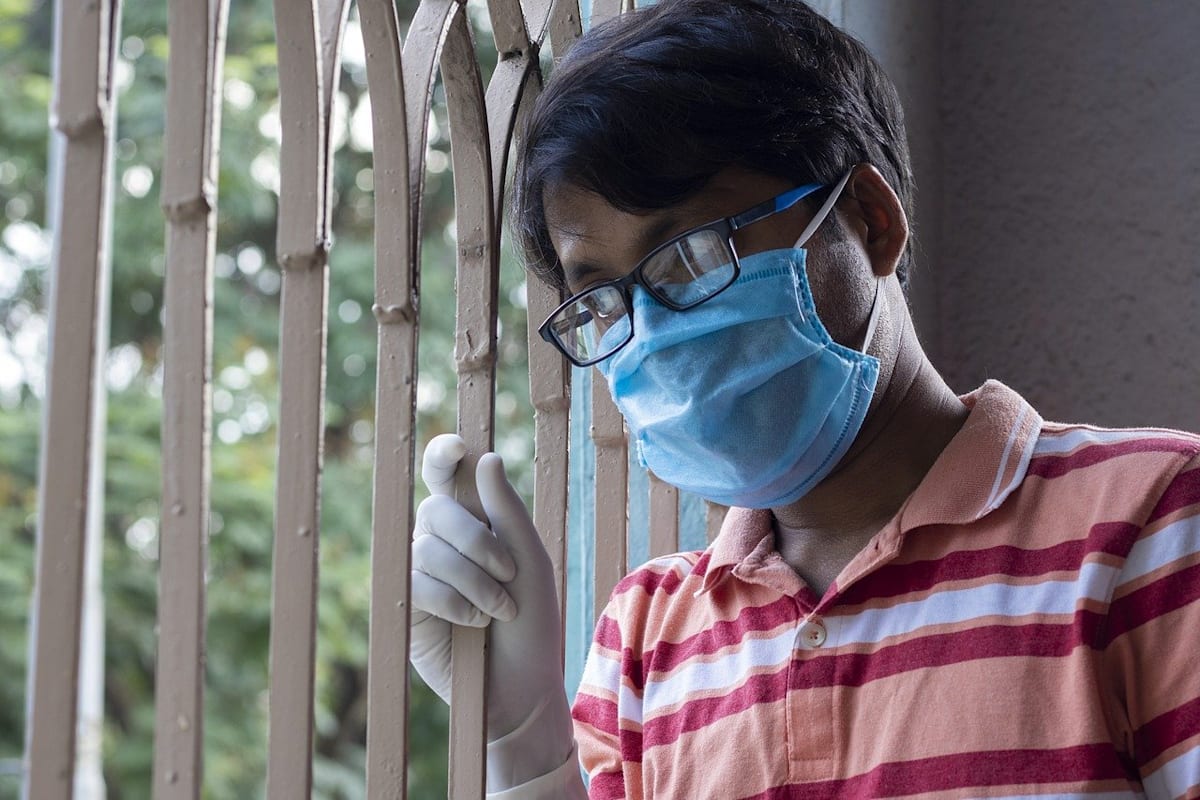
The anxiety associated with Covid disease, the economic burden, and the social distancing during Covid, all have produced psychological pressure on the overall population and especially on the vulnerable section of the population. Patients with chronic pain are vulnerable section and that they are suffering a ton. Pain Management in Covid is challenging for physicians too.
The pandemic caused by COVID-19 has resulted in the need for the overall public to isolate and maintain social distancing to prevent the spreading of the disease. This has resulted in a negative impact on the psychological state of chronic pain patients.
A survey administered by the Spanish Pain Society on 340 participants shows that 91.4% of people with chronic pain felt that the lockdown has affected their psychological state, and 63% complained that their quality of sleep was horrible compared to pre-pandemic time.
In another study published in Nature revealed that more anxiety and/or depression is related to more insomnia and pain in Covid time.
Why patients with chronic pain are feeling more pain in Covid time?
There is a vicious circle. Covid situation is producing more stress leading to anxiety and depression. Anxiety and depression are causing more pain. Pain produces more mental stress and there is a worsening psychological state. Study shows that there's worsening of physical and emotional health during Covid pandemic more due to isolation and social distancing. Pain and depression are very important long covid symptoms.
How to break the vicious cycle?
The cycle should be broken at different levels targeting both pain management and depression management. The following steps are proved and recommended.
Mental tricks: Stay connected with friends and relations with telephone, video calling, and social media; accept that anxiety is normal; distract yourself by engaging with favorite things like watching a movie, reading books, cooking, etc
Physical activities and exercises: Inactivities and rest cause deconditioning of muscles, joints, bone and increases pain. So movements in lifestyle activities must be done by chronic pain patients. Exercises also reduce depression. Thus movements of lifestyle activities and straightforward exercises like walking are encouraged to interrupt the cycle.
With the advice of doctors following medicines can be taken:
- Pain medicines: The of paracetamols, opioids, non-steroidal anti-inflammatory drugs, and corticosteroids in patients with COVID-19 to require care of pain.
- Depression medicines: Many antidepressants are used clinically to treat chronic pain particularly neuropathic pain. With proper doses, they will treat both pain and depression. Among these medicines, the foremost commonly used medicines are amitriptyline, venlafaxine, and duloxetine. Amitriptyline may be a tricyclic which will cause dryness of the mouth, constipation, orthostatic hypotension, arrhythmias, etc. Venlafaxine and duloxetine are serotonin and noradrenaline reuptake inhibitors and may also cause arrhythmias, constipation, GI upset, vertigo, dizziness, etc.
What is the take-home message?
Pain and mental disease are strongly associated and they coexist in more than 50% of situations. Both deteriorations of psychological health and increase of pain are found in patients of chronic pain in Covid time. Physical activities, exercises, staying connected with friends, engaging in favorite hobbies can all help in reducing morbidity. Pain medicines and antidepressant medicines should be taken when needed with the recommendation of physicians.
Evelyn Patterson @ on — Edited @ on
Of course, all these factors can accumulate and play a cruel joke with us. Therefore, we need to immediately pay attention to the state of anxiety and accumulated problems. But sometimes problems can be deeply rooted and manifest over time. I felt this firsthand when I got confused in my preferences and desires. Online counseling for LGBT helped me understand myself. And thanks to this, I felt myself not so lonely and alien in this world.
Reply Report abuse
Oda Huel @ on
I have chronic pain and I thought it was just me until I met my doctor. It's not that he didn't care about me, but he was so busy with other patients that he couldn't help me. So I had to find another doctor. You can download nursing templates through this https://masterbundles.com/templates/presentations/powerpoint/nursing/ site. I've been seeing a new one for about a year now and she's great! She listens to my problems and treats them accordingly. She also has a good sense of humor which helps relieve some of the stress of having chronic pain.
Reply Report abuse